Care for OCD That Respects Your Experience
Fullarton Clinic, provides comprehensive care that helps reduce Obsessive Compulsive Disorder symptoms and restore confidence.
OCD goes far beyond the stereotype of being “clean” or “organised.”
It’s a mental health condition that can feel intrusive, exhausting, and isolating.
Understanding Obsessive Compulsive Disorder (OCD)
OCD involves unwanted, intrusive thoughts (obsessions) and repetitive actions (compulsions) aimed at easing distress. These patterns can interfere with work, relationships, and daily life — often causing deep emotional discomfort.
Research from Swinburne University’s Centre for Mental Health and Brain Sciences indicates that OCD commonly emerges around the age of 19. Depression and Anxiety are often associated with OCD; however, with expert support, many people experience meaningful relief and learn strategies to manage their symptoms more effectively.

OCD is not a personality quirk — it’s a recognised and treatable condition.
Understanding the Difference Between OCD and OCPD
OCPD (Obsessive-Compulsive Personality Disorder) and OCD (Obsessive-Compulsive Disorder) are often confused because of their similar names, but they are distinct mental health conditions. OCD is an Anxiety-related disorder involving unwanted intrusive thoughts and repetitive conduct aimed at reducing distress. In contrast, OCPD is a personality disorder characterised by rigid thinking patterns, perfectionism, and an overwhelming need for control — often seen as appropriate or even beneficial by the person experiencing it.
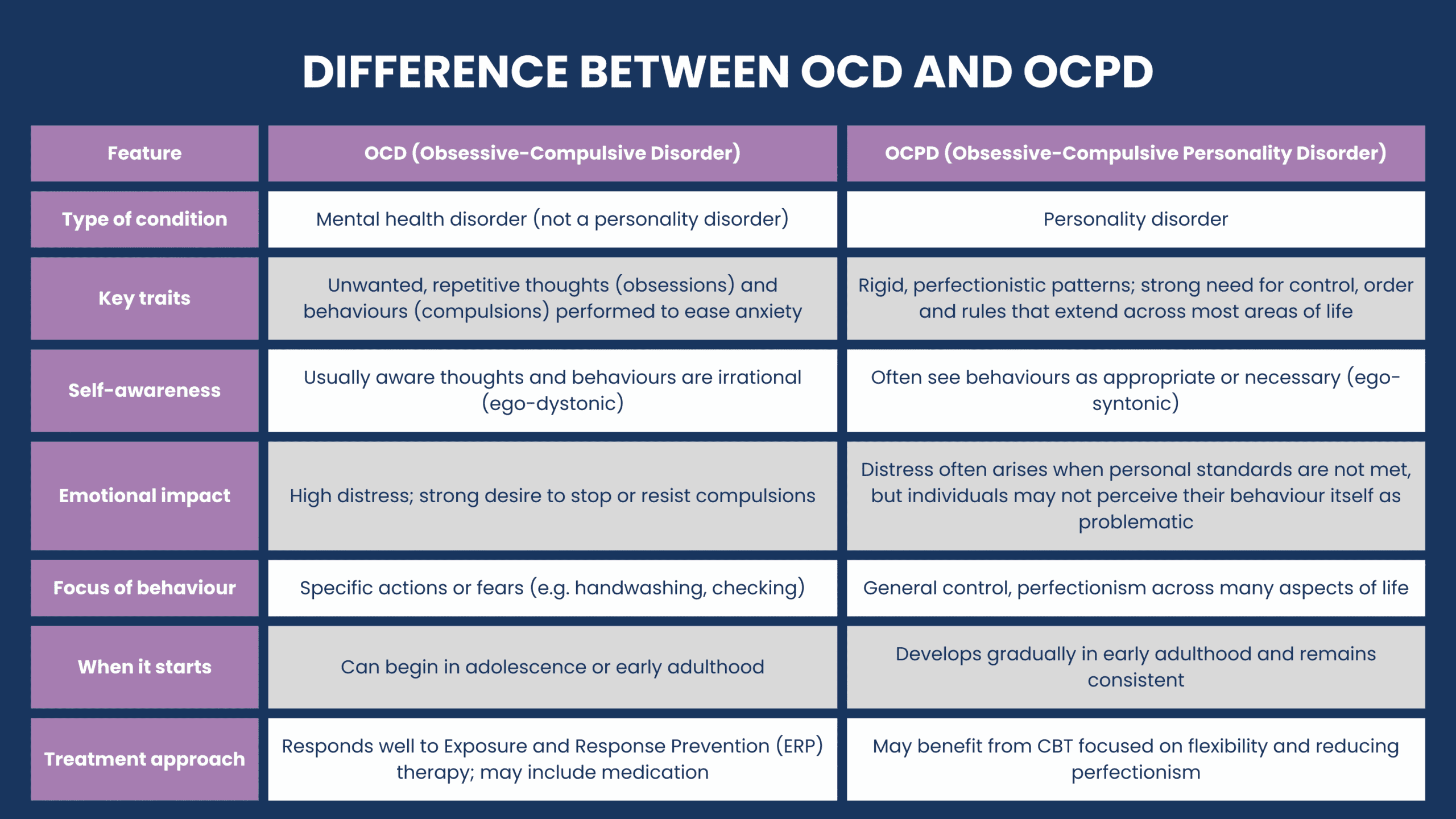
- People with OCD are typically aware that their obsessions and compulsions are irrational and unwanted.
- Those with OCPD usually believe their need for order and control is justified or necessary, which may make them less inclined to seek help.
- OCD tends to cause significant internal distress and interferes with specific aspects of life.
- The impact of OCPD symptoms is often broader and more ongoing — it influences the person's overall personality, how they interact in relationships, work, and daily functioning.
- OCD typically responds well to Exposure and Response Prevention (ERP), while OCPD may benefit more from therapies that focus on flexibility, interpersonal insight, and perfectionism.
Whether your symptoms are new or something you’ve managed for years, compassionate, evidence-based care is available — and can help you find relief and regain control.

Signs You May Need Support
You might benefit from specialist care if you are experiencing these OCD symptoms.
- Repetitive, distressing thoughts that feel intrusive or hard to control
- Compulsions such as checking, handwashing, counting, or repeating actions
- Fear or preoccupation that something bad will happen if you don’t perform certain rituals
- Avoidance of people, places, or responsibilities due to OCD-related Anxiety
- Feelings of shame, overwhelm, or exhaustion related to your thoughts or behaviour
OCD affects around 2–3% of Australians (approximately 500,000 people).
It often takes years to receive a diagnosis — but with the right help, change is possible.
Support can make a real difference.
With the right care, OCD can become more manageable — and life can feel less restricted.

Your Mental Health Support Starts Here
Our team at Fullarton Clinic offers personalised Obsessive Compulsive Disorder Treatment in a safe, structured environment, with Mental Health Programs designed to meet your needs.
1
Personalised OCD Care
Comprehensive Psychiatric and Psychological assessment to understand your unique experience. Your treatment plan is then tailored to your needs while guided by evidence-based therapies.
2
High Quality Treatment
Cognitive Behavioural Therapy (CBT) combined with Exposure and Response Prevention (ERP) — the gold-standard therapy for OCD. This approach is proven to reduce symptoms and help you regain control.
3
Pharmacy Services
Where clinically appropriate, medication can help reduce the physical symptoms of OCD and improve daily functioning.
4
Comprehensive Therapy
Individual and group therapy to build tools to manage intrusive thoughts and develop strategies to navigate daily life with greater ease.
5
Ongoing Monitoring and Support
Regular reviews ensure your care plan remains responsive to your progress and needs, and we adapt your care as you grow in confidence and stability.
6
Coordinate with Your Team
We work with your GP, Psychologist, or Psychiatrist to ensure seamless communication and continuity of care.
7
Dual Diagnosis Support
Identifying and treating coexisting medical conditions.
8
Screening for Chronic Disease
While staying with us, you will be screened and treated for other chronic diseases impacting your overall health.
9
Aftercare Support
Structured Day Programs and discharge planning help you maintain progress and support long term recovery.
Together, these nine components reflect our complete care model.
Which is designed to support you and promote long term wellbeing as you live with OCD.
Additional Treatment Options for OCD
We recognise that OCD may overlap with other challenges, such as:
- Anxiety and Mood Disorder Programs – For coexisting mental health conditions
- Explore our Mental Health Programs
-
Addiction Recovery Support – When substance misuse is part of the picture, Fullarton Clinic offers cohesive Dual Diagnosis support.
Explore our Addiction Recovery Program
Frequently Asked Questions
Getting help doesn't mean failing; you're finally being seen.
When a Steady Environment Helps You Feel More Like Yourself
When life feels overwhelming and it’s hard to get through the day, having a calm and structured setting can make a real difference. It can give you the space to better understand OCD and start moving forward.
At our private Mental Health Hospital, you’ll find spacious rooms with ensuites, plenty of natural light, and supportive shared spaces — all thoughtfully designed to help reduce distress and support your wellbeing.
Learn how Fullarton Clinic can support your healing and help you live more freely with OCD.
Explore our Mental Health Services
Our dedicated mental health hospital in Epping offers both Inpatient and Outpatient Programs in Melbourne’s northern suburbs.

OCD healing starts with expert care.
Our Inpatient Program provides structured support to help manage Obsessive Compulsive Disorder symptoms, improve functioning, and reduce overwhelm.

Stay supported and stay on track — our Day Programs are here to help you continue progressing after completing Inpatient care.
Receive ongoing mental health support in the same safe and familiar hospital environment.
