Structured Care for Those Who Struggle to Let Go of Control
Fullarton Clinic offers structured support to help you manage OCPD and live with greater balance, flexibility, and connection.
Understanding Obsessive-Compulsive Personality Disorder (OCPD)
OCPD is a long-standing personality pattern that can cause emotional strain, relationship difficulties, and burnout.
It is defined by a need for order, control, and perfection that goes beyond productivity or discipline.
People with OCPD may feel deeply anxious when routines are disrupted, struggle to delegate, or be extremely self critical.
Unlike OCD, which involves distressing thoughts and compulsive behaviours, OCPD is a pervasive personality style. It can affect how a person thinks, relates, and functions across many areas of life.

With structured support, individuals with OCPD can build emotional flexibility, improve relationships, and reduce the impact of rigid patterns.
OCPD is one of the most common personality disorders globally.
Some research suggests rates as high as 6.5% in the general population.
Support can make a real difference. With the right care, OCPD can become more manageable — and life can feel less rigid.

Signs You May Need Support
If you are experiencing these OCPD symptoms, you may benefit from support:
- Intense discomfort when routines are disrupted or things feel out of control
- Excessive focus on work, productivity, or rules — sometimes at the expense of rest or relationships
- Difficulty trusting others to help or struggling to delegate tasks
- High levels of self criticism or perfectionism behaviours
- Strained relationships due to unrealistic standards or emotional rigidity
OCPD often goes undiagnosed, as traits may be mistaken for ambition or diligence.
But when these patterns cause distress, support is available.
Understanding the Difference Between OCD and OCPD
Although their names sound similar, Obsessive-Compulsive Personality Disorder (OCPD) and Obsessive-Compulsive Disorder (OCD) are distinct mental health conditions. OCPD is a personality style shaped by strong patterns of control, perfectionism, and a rigid approach to rules and order. The table below details how it differs from OCD, which is an anxiety related condition involving intrusive, unwanted thoughts and compulsions that aim to relieve distress.
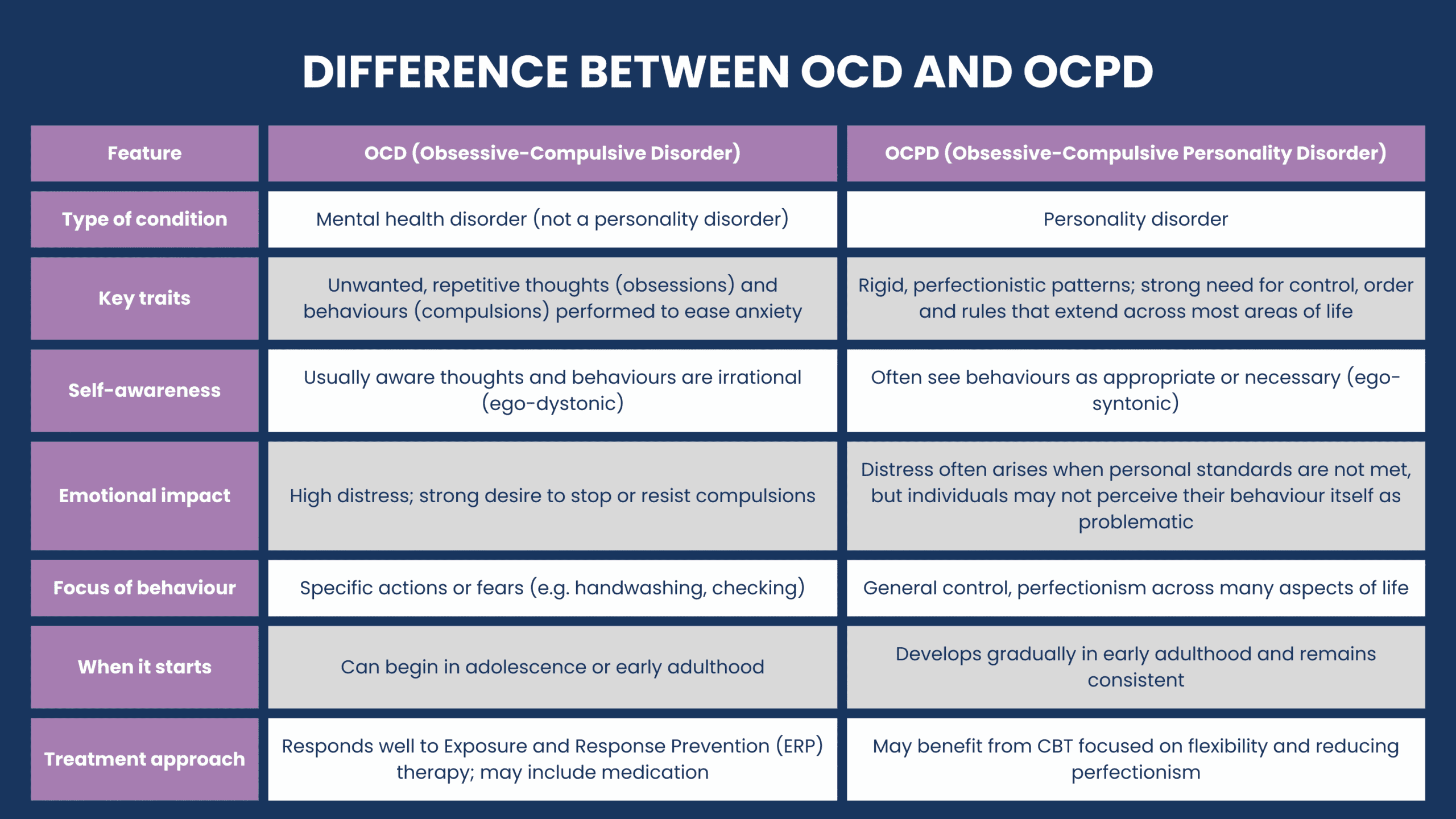
- People experiencing symptoms of OCPD usually believe their need for order and control is justified or necessary, which may make them less inclined to seek help.
- The impact of OCPD symptoms is often more pervasive — it influences the person's overall personality and how they interact in relationships, work, and daily functioning.
- OCPD may benefit more from therapies that focus on flexibility, interpersonal insight, and perfectionism.
Support through therapy can help you identify these patterns, understand their underlying causes, and learn more flexible, adaptive ways of thinking and behaving.
Perfectionism Behaviours in OCPD
Perfectionist patterns are often a core aspect of Obsessive-Compulsive Personality Disorder (OCPD).
While striving for improvement and excellence at tasks that are important to you, perfectionism in OCPD tends to be rigid and excessive. This can interfere with your daily functioning, relationships, and overall wellbeing.
This is sometimes called maladaptive perfectionism, where:
- Your expectations on yourself are often unachievable
- You view your mistakes as personal failures
- You may delay tasks for fear of not doing them perfectly
- You may struggle with delegation and or may spend excessive time on small or unimportant details.
Over time, these behaviours can lead to:
- Increased stress and burnout, and trouble at work
- Tension in your personal relationships.


Your Mental Health Support Starts Here
Our team at Fullarton Clinic offers personalised Obsessive Compulsive Personality Disorder care in a safe, structured setting. Your treatment plan is tailored to your unique experience, goals, and preferences.
1
Tailored Assessment
Comprehensive psychiatric and psychological evaluation to understand how OCPD patterns affect your life and relationships.
2
Evidence-Based Therapy
Cognitive and interpersonal therapies that help you manage control-oriented thinking, perfectionism, and emotional restriction.
3
Pharmacy Services
Where clinically appropriate, medication can help reduce the physical symptoms of OCPD and improve daily functioning.
4
Therapeutic Community
Including individual counselling, group therapy, and holistic wellness programs such as physical activity and creative therapies — supporting OCPD resolution through both emotional and physical engagement.
5
Ongoing Monitoring and Support
Regular reviews ensure your care plan adapts to your evolving needs throughout treatment.
6
Coordinate with Your Team
We work with your GP, Psychologist, or Psychiatrist to ensure seamless communication and continuity of care.
7
Dual Diagnosis Support
Identifying and treating coexisting medical conditions.
8
Screening for Chronic Disease
While staying with us, you will be screened and treated for other chronic diseases impacting your overall health.
9
Aftercare Support
Structured Day Programs and discharge planning help you maintain progress and reduce relapse risk.
Together, these nine components reflect our complete care model—designed to support lasting symptom management and promote sustained wellbeing during your experience living with OCPD.
Additional Treatment Options for OCPD
We recognise that OCPD may overlap with other challenges, such as:
-
Anxiety and Mood Disorder Programs – For coexisting mental health conditions.
Explore our Mental Health Programs -
Addiction Recovery Support – When substance misuse is part of the picture, Fullarton Clinic offers cohesive Dual Diagnosis support.
Explore our Addiction Recovery Program
Experienced clinicians in our supportive, private hospital setting oversee your care throughout the program.
Frequently Asked Questions
Seeking help for Obsessive Compulsive Personality Disorder takes courage.
At Fullarton Clinic, you won't be judged.
You'll be welcomed with respect, supported by an experienced team, and offered care that recognises the complexity of your experience.
When a Steady Environment Helps You Feel More Like Yourself
If you’re struggling with OCPD symptoms day to day, a calm and structured setting can provide the stability needed to better understand your experience and move forward.
Our private Mental Health Hospital offers spacious rooms with ensuites, natural light, and supportive communal spaces — all thoughtfully designed to promote healing and wellbeing.
Learn how Fullarton Clinic can support your healing and help you live more freely with OCPD.
Explore our Mental Health Services
Our dedicated mental health facility in Epping offers both Inpatient and Outpatient Programs in Melbourne’s northern suburbs.

An improved experience of OCPD starts with expert care.
Our Inpatient Program provides structured support to help manage Obsessive Compulsive Personality Disorder symptoms, and live with greater balance, flexibility, and connection.

Stay supported and stay on track — our Day Programs are here to help you continue progressing after completing Inpatient care.
Receive ongoing mental health support in the same safe and familiar hospital environment.
